Denial Management Services
Our team ensures denied claims are corrected, compliant with payer requirements, and resubmitted promptly to maximize recovery.
Connect with us now
Recover Revenue, Improve Efficiency by Ascendant Medical
Claim denials are a major obstacle to a healthcare practice’s financial health, resulting in lost revenue and operational inefficiencies. Ascendant Medical offers comprehensive denial management services to identify, resolve, and prevent claim denials. Our goal is to help healthcare providers recover lost revenue and streamline their revenue cycle for sustained growth.

Clean Claim Rate
Compliance Guarantee
Faster Payments
We perform an in-depth analysis of denied claims to identify trends, root causes, and recurring issues, enabling targeted solutions to prevent future denials.
Our team ensures denied claims are corrected, compliant with payer requirements, and resubmitted promptly to maximize recovery.
We liaise with insurance payers to address claim issues, clarify requirements, and resolve disputes efficiently, ensuring timely reimbursements.
By analyzing denial patterns and educating your team, we implement preventive measures to reduce denial rates and improve first-pass claim approvals.

Expertise in Denial Resolution
Our team of specialists has extensive experience in addressing denials across all specialties and payer types.

Tailored Solutions
We customize our approach to meet the unique needs of your practice, ensuring maximum efficiency and effectiveness.

Commitment to Results
At Ascendant Medical, we prioritize recovering your revenue and optimizing your operations to achieve long-term success.
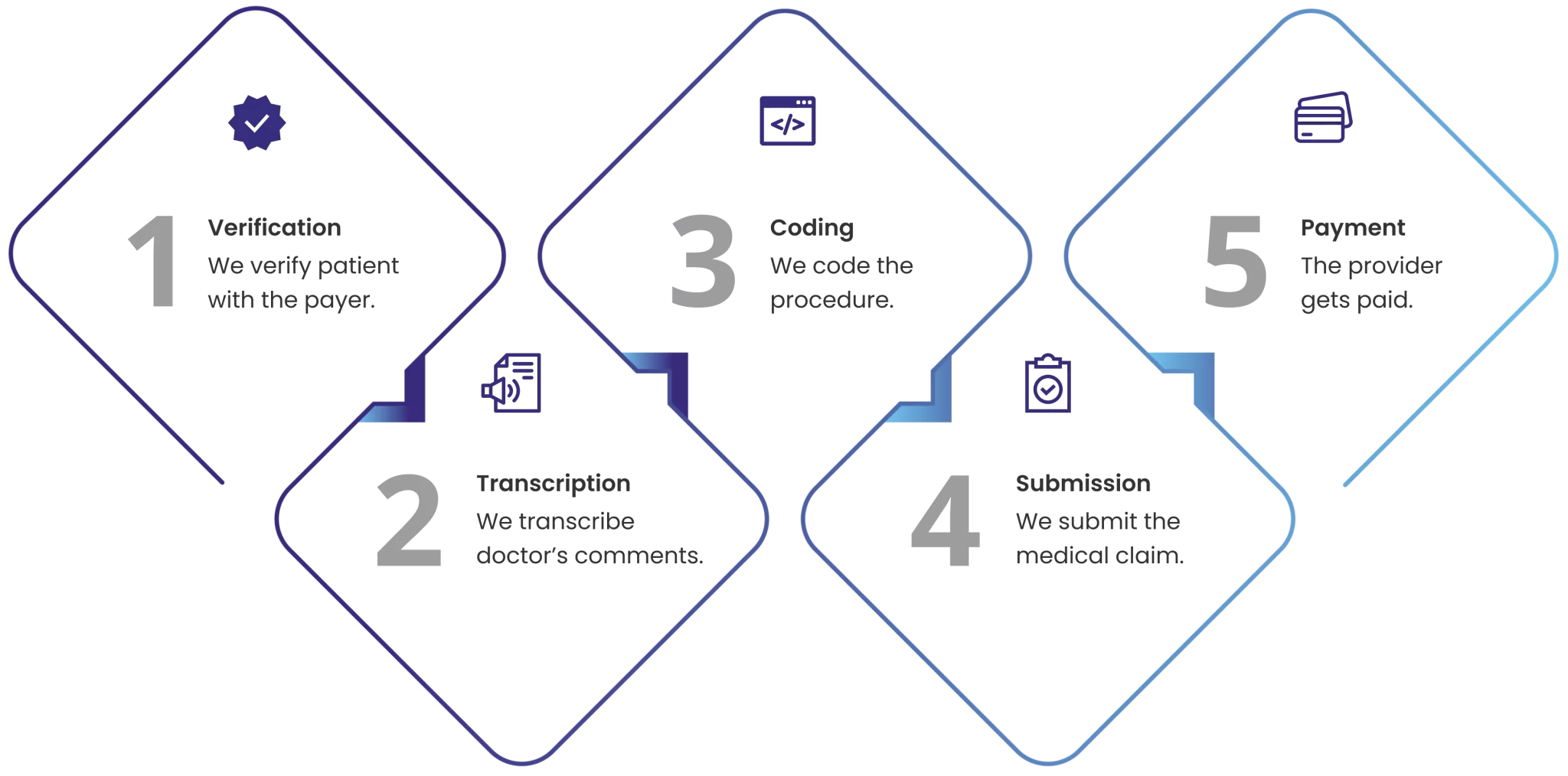
How Our Billing Process Works?

Don’t let denials impact your practice’s bottom line.
Our experts investigate the reasons behind denials, such as coding errors, missing information, or non-compliance with payer rules. We implement training and process adjustments to minimize future denials, improving claim accuracy and compliance. Denied claims are reviewed, corrected, and resubmitted promptly to maximize recovery rates.
%
Clean Claim Rate Approval
%
Fast Reimbursements
%
Payer-Provider-Patient Satisfaction
%
Compliance Guarantee
Ascendant Medical can maximize your ROI.
Expert analysis and opinions on everything related to Health IT
Comparing Ascendant Medical's Credentialing Efficiency...
Table Of Contents: Comparing AR Recovery Services:...
Top Common Mistakes to Avoid When Accurately Reviewing...
Frequently Asked Questions
How can Ascendant Medical help my practice?
How do you ensure compliance with healthcare regulations?
What is denial management, and how does it benefit my practice?
How do you handle aged claims collections?
Can you provide customized reporting?
How can I get started with Ascendant Medical?